Clara Health
Overview of Clara Health
What is Clara Health?
Clara Health is an innovative AI-powered platform designed specifically for healthcare providers to uncover and recover hidden revenue opportunities buried in call recordings and Electronic Medical Records (EMR). In the fast-paced world of home care, hospice, and other medical services, revenue leaks often occur due to missed documentation, unclaimed shifts, or billing errors during patient interactions. Clara Health steps in as your AI co-pilot, analyzing vast amounts of data from phone calls, voicemails, emails, and EMR entries to pinpoint these issues. By deploying specialized AI agents—like intake specialists, payroll experts, and compliance officers—it automates the recovery process, ensuring no dollar slips through the cracks. Trusted by top healthcare providers, this tool transforms overlooked conversations into tangible financial gains, helping organizations scale efficiently while maintaining compliance.
Core Features of Clara Health
At its heart, Clara Health offers a suite of domain-tuned AI agents that handle repetitive, revenue-impacting tasks. Here's a breakdown of its key capabilities:
Call and EMR Transcription & Analysis: The platform transcribes every inbound and outbound phone call, voicemail, SMS, and email in real-time. It then cross-references this data with EMR details, such as visit notes, claims, and billing records, to identify discrepancies like missing signatures on timesheets or unverified shifts.
Specialized AI Agents: Customize agents for roles including AI Coordinator, Intake Specialist, Payroll Specialist, Data Analyst, Customer Service Rep, Compliance Specialist, Onboarding Specialist, and Authorization Specialist. For instance, a Billing Agent can automatically follow up on payor documentation, while an HR Agent checks payment statuses and resolves tickets.
Omni-Channel Integration: Supports seamless connectivity across phone calls, SMS, email, and EMR systems. It integrates with popular tools like HHAeXchange, PBX/VOIP software, CRM systems, and various EMR platforms, ensuring broad compatibility without requiring extensive engineering from your side.
Task Tracking and Automation: AI agents not only spot issues but also execute actions—such as resubmitting claims or filling shifts—and track progress via a live dashboard. Built-in testing ensures reliability, with features like in-call guardrails to maintain safety, anti-toxicity measures, and script adherence.
Multilingual Support: Handles conversations in multiple languages, making it ideal for diverse patient populations. For example, it can respond in English while blocking sensitive topics to uphold compliance.
These features make Clara Health a powerhouse for revenue cycle management in healthcare, reducing manual workloads and boosting bottom lines.
How Does Clara Health Work?
Clara Health operates through a streamlined, three-phase process that minimizes disruption while maximizing results. Understanding its workflow can help you see why it's a game-changer for busy healthcare teams.
Phase 1: Assessment and Integration
The journey begins with a tailored assessment where Clara's team integrates directly with your existing contact center software, VOIP systems, and EMR. They quantify revenue leaks—such as unclaimed visits or delayed authorizations—by analyzing historical data. You'll receive a custom AI menu outlining potential fixes, like deploying an AI Payroll Specialist to handle timesheet issues. This phase typically takes 1-3 weeks, with no extra costs for custom integrations; Clara's engineers collaborate with your IT and vendors to build what's needed.
Phase 2: Implementation and Fine-Tuning
Once assessed, an dedicated engineer works alongside your team to deploy and fine-tune AI agents. This includes setting up omni-channel reach for inbound/outbound communications and EMR-aware actions that pull real-time data, such as visit histories or caregiver assignments. For example, if a call reveals a shift opening, the AI Intake Specialist can immediately notify available staff via SMS or email. Guardrails ensure ethical use: prompts are protected against injections, and topics are blocked to comply with HIPAA standards. Testing is rigorous—18 out of 18 scenarios passed in demos—guaranteeing smooth rollout.
Phase 3: Monitoring and Results
With agents live, recovered revenue starts flowing. Track everything on a intuitive dashboard: resolved tickets, filled shifts, collected payments, and overall wins. Staff only intervene for edge cases, like approving unusual claims. The AI runs autonomously post-setup, analyzing new data continuously to prevent future leaks. Data governance is top-notch—your information stays encrypted, never used for training external models, and fully HIPAA compliant.
This end-to-end automation not only recovers lost dollars but also enhances operational efficiency, from caregiver scheduling to payor follow-ups.
Primary Use Cases and Practical Value
Clara Health shines in scenarios where human oversight falls short due to volume or complexity. Consider these real-world applications:
Shift Filling and Caregiver Coordination: In home care agencies, an unexpected absence can mean lost billable hours. Clara's AI detects openings from calls (e.g., "Hi Tina, an 8-hour shift just opened") and assigns coverage via automated outreach, reducing no-show rates and maximizing revenue.
Billing and Claims Recovery: Missing patient signatures or incomplete docs lead to denied claims. The platform spots these in EMR-call pairings and deploys a Billing Agent to resubmit, following up with payors until resolution.
Compliance and Onboarding: Ensure all interactions adhere to regulations with AI Compliance Specialists that monitor calls for accuracy and handle new caregiver onboarding seamlessly.
Customer Service Enhancement: AI Customer Service agents manage inquiries in any language, from appointment rescheduling to payment status checks, freeing staff for high-value tasks.
The practical value is clear: healthcare providers using Clara Health report rapid ROI through reclaimed revenue—think thousands in missed shifts or claims per month. It scales with your business, supports growth without proportional staff increases, and provides peace of mind with robust security. In an industry facing tight margins, this tool turns data into dollars, improving both financial health and patient care delivery.
Who is Clara Health For?
This platform is tailored for healthcare organizations dealing with high-volume communications and documentation, including:
Home Care and Hospice Agencies: Battling staffing shortages and billing complexities.
Medical Call Centers: Overwhelmed by inbound/outbound interactions.
Larger Providers with EMR Systems: Seeking to optimize revenue cycles without heavy IT investments.
If your team struggles with revenue leakage from calls or EMR gaps, Clara Health is ideal. It's especially valuable for non-technical users, as no ongoing engineering is required—just plug in and let AI handle the rest.
Why Choose Clara Health Over Alternatives?
Unlike generic AI tools, Clara Health is healthcare-specific, with domain-tuned agents that understand medical jargon, compliance needs, and revenue nuances. Its outcome-based pricing—platform fee plus per-successful-action billing—aligns costs with value, avoiding upfront risks. Plus, the dedicated support, from implementation managers to regular progress meetings, ensures a smooth experience. In testimonials from top providers, users highlight the ease of setup and immediate impact on lost revenue recovery.
Pricing and Setup Insights
Setup is quick: 1-3 weeks for the platform, slightly longer for complex agents. Pricing includes a base fee for data analysis and transcription, with AI actions billed per outcome (e.g., a filled shift or collected payment). No hidden fees for integrations, and full transparency via the dashboard.
Frequently Asked Questions
How Long Does Setup Take?
Expect 1-3 weeks for the core platform, with AI agents customized based on your needs. A dedicated manager guides you, including weekly check-ins.
What Data Is Analyzed?
All calls, voicemails, SMS, emails, and EMR data like visits, claims, and billing—transcribed and linked for quick insights.
Do We Need In-House Engineers?
No, Clara handles integrations. Post-setup, it's hands-off except for dashboard oversight.
How Is Data Protected?
HIPAA compliant with encryption, access controls, and no data sharing or model training. Your info stays yours.
Ready to rescue your revenue? Schedule a demo today and see how Clara Health can transform your operations. With events like product demos on February 4th, now's the time to integrate AI into your workflow for sustainable growth.
Best Alternative Tools to "Clara Health"
Gryphon AI empowers organizations to drive revenue growth and mitigate risks by balancing regulatory compliance and business objectives across marketing, sales, and customer service interactions.
FlyCode is an AI-powered platform that helps SaaS and eCommerce businesses recover failed payments and reduce involuntary churn, increasing subscription revenue through intelligent payment retries and optimization.
Resolvd automates complex reconciliation and execution workflows for healthcare and enterprise operations using AI-powered digital workers, reducing backlogs, contractor spend, and recovering lost revenue.
RevRag.AI provides AI agents for revenue teams, automating lead qualification, onboarding, and support. Designed for BFSI, Fintech, and Insurtech, it aims to boost conversions and improve customer engagement.
Keatext is an AI-powered text analytics platform that helps businesses analyze customer feedback from various channels to identify key insights, improve customer satisfaction, and drive business growth.
Hunchbank: AI-powered Stripe analytics to unlock more revenue from existing customers. Automate email marketing, prevent churn, detect fraud with AI agents.
Azna AI is an AI-powered rebooking system designed specifically for med-spas, helping recover lost revenue from clients who forget to schedule follow-up treatments through intelligent voice and SMS conversations.
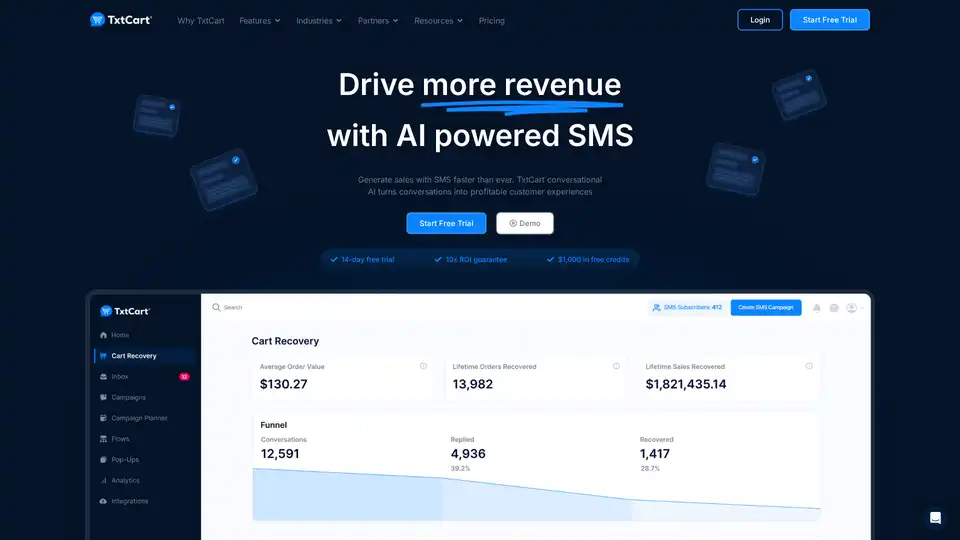
TxtCart is an AI-powered conversational SMS marketing platform for Shopify brands that turns visitors into profitable conversations with automated campaigns, cart recovery, and AI assistance.
Edgy Labs provides AI-powered SEO solutions to boost your online visibility and drive revenue. Specializing in generative engine optimization and technical SEO.
Slicker is a no-code AI platform that automates payment recovery for subscription businesses, using machine learning to detect and retry failed payments, reducing involuntary churn and maximizing recurring revenue with seamless integrations.
ONVY is an AI-driven health intelligence platform that integrates 500+ data sources for hyper-personalized health coaching, boosting user engagement and business insights in wellness apps.
AppBuzz is an AI-powered no-code mobile app builder for Shopify, WooCommerce, BigCommerce, and Wix stores. Create free, low-cost apps with real-time syncing, push notifications, and abandoned cart recovery to boost conversions up to 5x.
Automate calls with OneAI's AI phone call agent, qualifying leads, booking meetings, and driving revenue across phone, SMS, and WhatsApp. Fast setup, full integration.
Oatmeal Health revolutionizes early cancer detection with AI-driven screening and navigation, empowering FQHCs and hospitals to improve care in underserved communities.